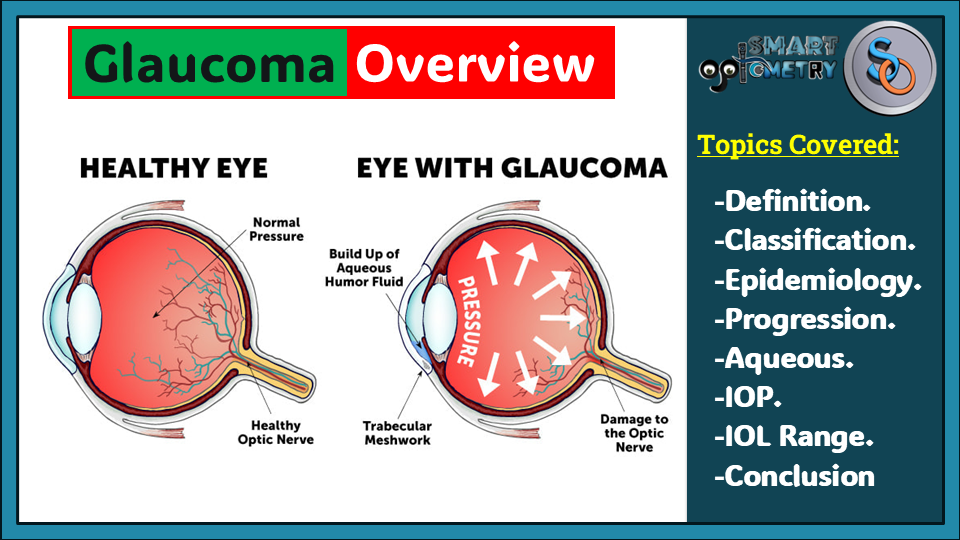
What is Glaucoma?
Glaucoma refers to a group of chronic progressive optic neuropathies characterized by structural changes in the optic nerve head and retinal nerve fiber layer, leading to retinal ganglion cell loss and visual field defects. Elevated intraocular pressure (IOP) is a key modifiable risk factor.
What is the Goal of Treatment?
The primary goal is to slow disease progression to maintain visual function and quality of life throughout the patient’s lifetime at a sustainable cost.
What is Classification of Glaucoma?
- Congenital or Acquired: Based on onset.
- Open-Angle vs. Angle-Closure: Differentiated by aqueous outflow mechanism and anterior chamber angle configuration.
- Primary vs. Secondary: Secondary glaucoma is associated with an identifiable ocular or systemic cause of IOP elevation.
What is the Epidemiology of Glaucoma?
- Affects 2–3% of individuals over 40, with up to 50% undiagnosed.
- Second leading cause of global blindness.
- Primary Open-Angle Glaucoma (POAG): Most common in whites, Hispanics/Latinos, and Blacks (highest prevalence in Blacks).
- Primary Angle Closure (PAC): Accounts for up to half of cases worldwide, with higher prevalence in Asians and newly recognized higher rates in whites under dark gonioscopy conditions.
.
.
What is the Progression of Glaucoma?
The Early Manifest Glaucoma Trial (EMGT) documented progression rates using visual field deterioration:
- High-Tension Glaucoma (HTG): −1.31 dB/year.
- Normal-Tension Glaucoma (NTG): −0.36 dB/year.
- Pseudoexfoliation Glaucoma (PXEG): −3.13 dB/year.
Without treatment, average visual function declines from normal to blindness over ~25 years, with IOP-lowering interventions significantly slowing progression.
Aqueous Humor Dynamics
Source of Aqueous Humor:
- Ciliary epithelium of the ciliary body (pars plicata).
Mechanism of Aqueous Humor Production:
- High-protein filtrate undergoes ultrafiltration through fenestrated capillaries.
- Active solute transport across ciliary epithelium establishes an osmotic gradient, facilitating passive water flow into the posterior chamber.
.
.
Regulation of Aqueous Humor:
- Sympathetic Nervous System in Aqueous Humor Production:
- Beta-2 receptors: Increase secretion.
- Alpha-2 receptors: Decrease secretion.
- Key enzyme associated with of Aqueous Humor Production:
- Carbonic anhydrase.
Aqueous Outflow/Drainage Anatomy:
1. Trabecular Meshwork in Aqueous Humor Outflow/Drainage:
- Sieve-like structure at the anterior chamber angle.
- Components:
- Uveal meshwork: Innermost, large spaces, minimal resistance.
- Corneoscleral meshwork: Middle, smaller spaces, moderate resistance.
- Juxtacanalicular meshwork: Outer, narrow spaces, major resistance.
2. Schlemm Canal in Aqueous Humor Outflow/Drainage:
- Circumferential channel in the perilimbal sclera.
- Inner wall: Giant vacuoles for aqueous transport.
- Outer wall: Collector channels connect to episcleral veins.
.
.
Aqueous Outflow/Drainage Physiology:
- Aqueous Outflow/Drainage Pathways:
Trabecular outflow (90%) of Aqueous Humor:
- Bulk flow through trabeculum → Schlemm canal → Episcleral veins (pressure-sensitive).
Uveoscleral drainage (10%) of Aqueous Humor:
- Across the ciliary body face → Suprachoroidal space → Venous circulation.
Iris outflow of Aqueous Humor:
- Minor aqueous drainage via the iris.
Intraocular Pressure (IOP):
What is Intraocular Pressure (IOP)?
- IOP is determined by the balance between aqueous production and aqueous outflow.
- Outflow resistance is influenced by the trabeculum and episcleral venous pressure.
What is Normal Intraocular Pressure (IOP) range?
- Upper limit: 21 mmHg (measured by applanation tonometry).
- Glaucoma can occur with IOP < 21 mmHg (normal-tension glaucoma) or may not occur with higher IOP (ocular hypertension).
.
.
Key Factors Influencing Glaucomatous Damage:
Optic Nerve Susceptibility:
- Blood supply integrity.
- Structural vulnerability to mechanical stress at the optic nerve head.
IOP Reduction:
- A central modifiable factor in glaucoma management, regardless of baseline IOP.
Fluctuations in Intraocular Pressure (IOP):
- Normal fluctuations depend on:
- Time of day: Higher in the morning, lower in the afternoon/evening (linked to diurnal variations in aqueous production).
- Heartbeat, blood pressure, and respiration.
- Glaucomatous eyes: Greater-than-normal fluctuations increase the risk of progressive visual field damage.
- A single IOP reading may be misleading; note the time of measurement.
.
.
Tags:
glaucoma overview, definition of glaucoma, chronic optic neuropathies, optic nerve head damage, retinal nerve fiber loss, visual field defects, elevated intraocular pressure, IOP risk factor, glaucoma treatment goals, types of glaucoma, open-angle glaucoma, angle-closure glaucoma, primary vs secondary glaucoma, congenital glaucoma, acquired glaucoma, global blindness causes, epidemiology of glaucoma, primary open-angle glaucoma prevalence, primary angle closure glaucoma, Asian glaucoma prevalence, natural history of glaucoma, glaucoma progression rates, high-tension glaucoma, normal-tension glaucoma, pseudoexfoliation glaucoma, aqueous humor dynamics, aqueous production, ciliary body function, trabecular meshwork anatomy, schlemm canal role, aqueous outflow pathways, trabecular outflow, uveoscleral drainage, intraocular pressure definition, normal IOP range, glaucomatous damage factors, optic nerve susceptibility, IOP fluctuations, diurnal IOP variations, morning IOP changes, IOP and visual field damage, ocular hypertension, normal-tension glaucoma, IOP reduction in glaucoma, glaucoma management,
- Check Our Courses: Ophthalmic Instrumentation, Clinical Refraction, Contact Lens, Binocular Vision, Dispensing Optics, MCQs in Optometry
- Download our App “Optometry Notes & MCQs” from Google Play Store.


2 Comments
We will continue posting blog about Glaucoma. Stay with us.
Part-2: Ocular Hypertension is already posted.
Check here:https://smartoptometryacademy.com/ocular-hypertension-oht/
I would like to know more about the topics.