What is Blepharitis?
- Blepharitis is a subacute or chronic inflammation of the eyelids.
- It’s extremely common, affecting both eyes and often seen in children.
What are the Causes of Blepharitis?

It’s typically caused by irritants like cosmetics, dust, or smoke and sometimes uncorrected refractive errors, where children rub their eyes for clear vision, leading to blepharitis. Parasitic infestations like Demodex folliculorum and Phthirus pubis can also be factors.”
- 1. Cosmetics, Dust & Smoke:
- These irritants cause inflammation and disrupt the normal tear film, leading to chronic irritation of the eyelid margins, which triggers blepharitis.
- 2. Uncorrected Refractive Error:
- When vision is blurred, children may frequently rub their eyes to try to see more clearly, causing repeated mechanical irritation that leads to Blepharitis.
- 3. Parasites- Like Demodex folliculorum and Phthirus pubis:
- These parasites infest the eyelash follicles and glands, causing irritation and inflammation as the body reacts to their presence, which leads to blepharitis.
.
.
What are the types of Blepharitis:
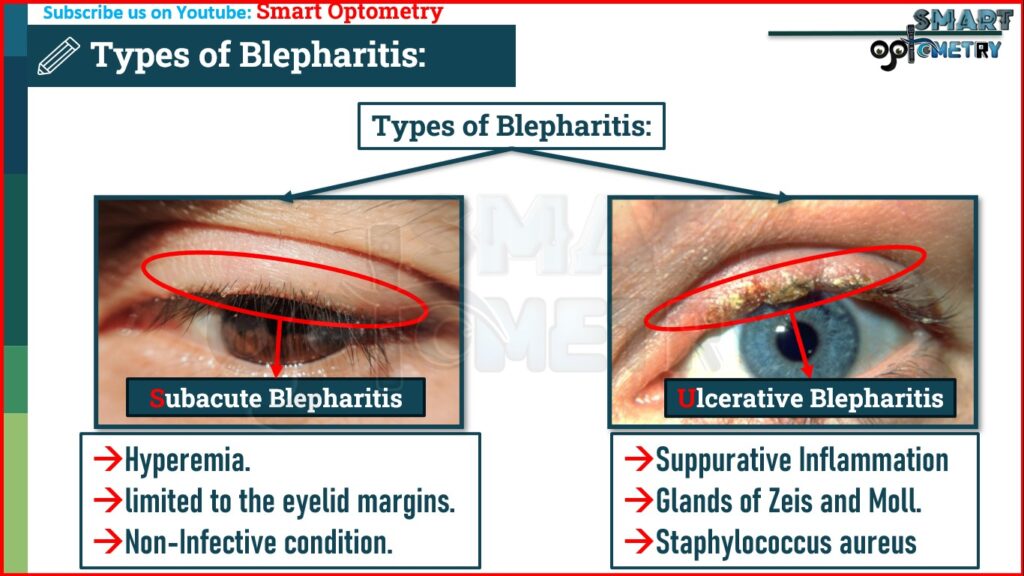
- There are two main types of blepharitis that we need to understand:
1. Squamous Blepharitis.
- It is characterized by hyperemia, usually limited to the eyelid margins. It is not an infective condition.
2. Ulcerative Blepharitis.
- It is caused by acute or chronic suppurative Inflammation of the follicles of the eyelashes and glands of Zeis and Moll. Staphylococcus aureus is usually the causative agent superimposed on predisposing conditions.
.
.
What are the Clinical Features of Blepharitis:
Symptoms of Squamous Blepharitis:
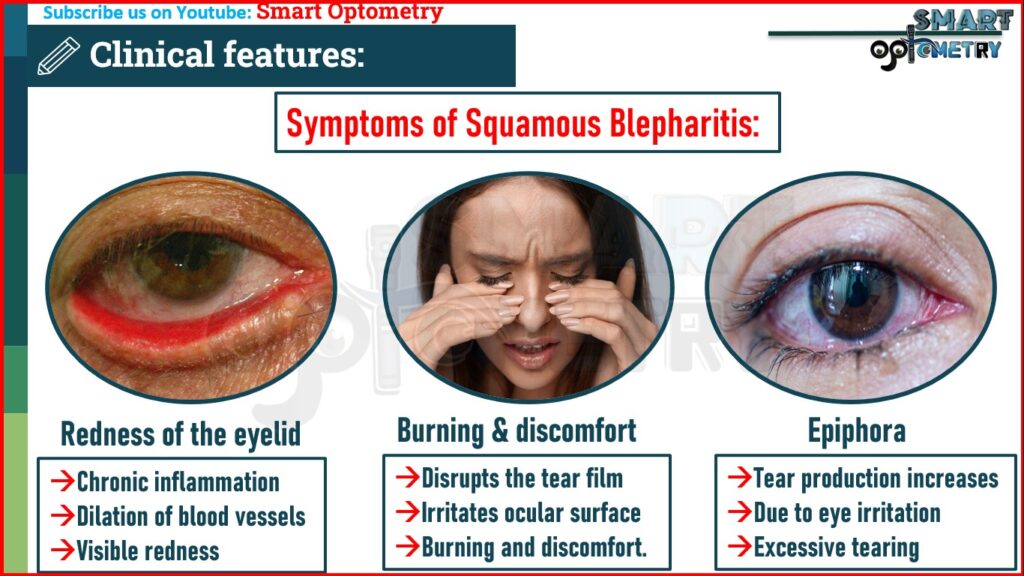
- Redness of the eyelid margins:
- Chronic inflammation causes dilation of blood vessels, leading to visible redness along the eyelid edges.
- Burning and discomfort of the eyes:
- Inflammation disrupts the tear film and irritates the ocular surface, leading to sensations of burning and discomfort.
- Epiphora:
- Tear production increases as a response to eye irritation, leading to excessive tearing or epiphora.
Symptoms of Ulcerative Blepharitis:
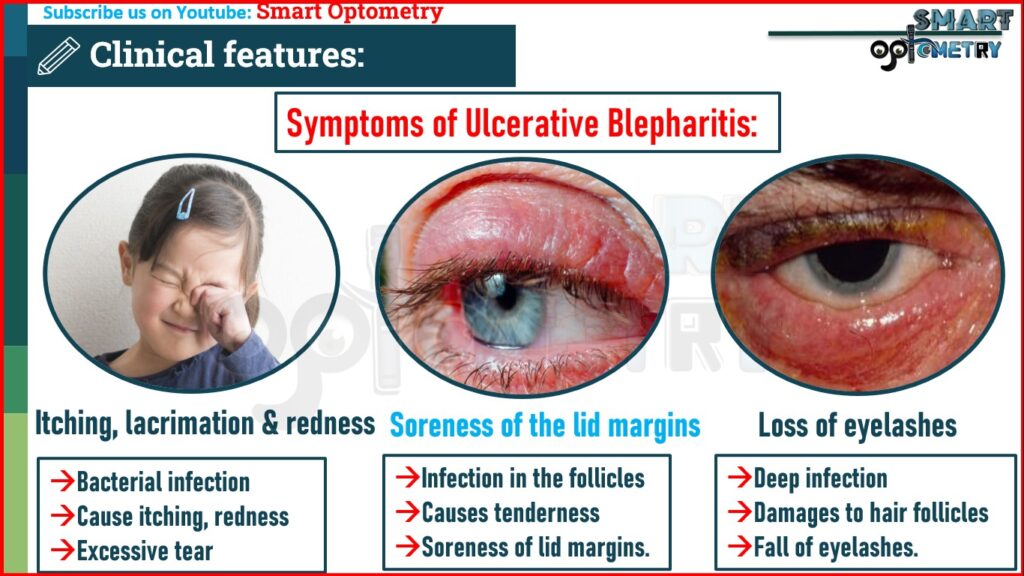
- Itching, lacrimation, and redness:
- Bacterial infection and inflammation cause itching, redness, and stimulate excessive tear production due to irritation.
- Soreness of the lid margins:
- Infection in the follicles and glands of the eyelid causes tenderness and soreness along the margins.
- Loss of eyelashes:
- Deep infection damages the hair follicles, leading to the fall of eyelashes.
.
.
Signs of Squamous Blepharitis:
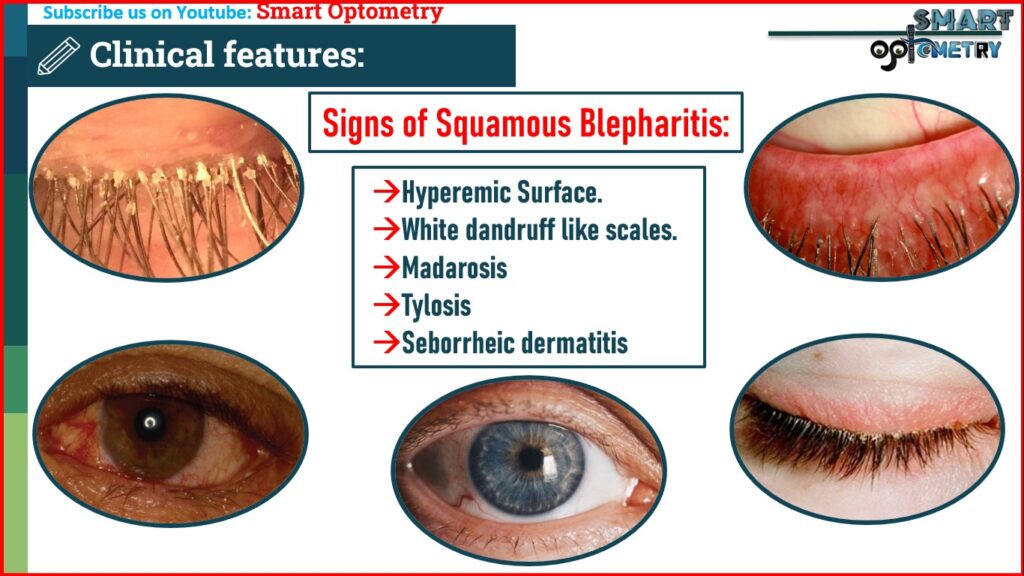
- White dandruff-like scales on the lid margins:
- Abnormal shedding of skin cells in chronic inflammation leads to the formation of flaky, dandruff-like scales along the lid margin.
- Hyperemic underlying surface:
- When scales are removed, the underlying tissue shows redness due to inflammation but remains intact without ulceration.
- Madarosis (Falling of the eyelashes):
- Chronic inflammation damages hair follicles, resulting in the gradual loss of eyelashes.
- Tylosis (Thickening of the lid margins):
- Persistent inflammation causes hypertrophy and thickening of the eyelid margins as a defense mechanism.
- Associated seborrheic dermatitis of the scalp:
- Blepharitis often coexists with seborrheic dermatitis, a condition that affects areas with oil-producing glands, including the scalp.
Signs of Ulcerative Blepharitis:

- Yellow crusts with matting at the roots of the eyelashes:
- Bacterial infection produces purulent material that forms yellow crusts, which stick the eyelashes together.
- Madarosis:
- Crusts adhere tightly, and their removal can pull out affected eyelashes lead to Madarosis.
- Bleed easily:
- Bacterial infection in hair follicles leads to ulcer formation; these bleed due to inflammation and vascular damage.
- Loss of cilia with misdirected growth:
- Repeated infection and healing cause scarring and abnormal cilia alignment or direction due to tissue contraction.
.
.
What is the Treatment of Blepharitis:
1. Treatment of Squamous blepharitis:
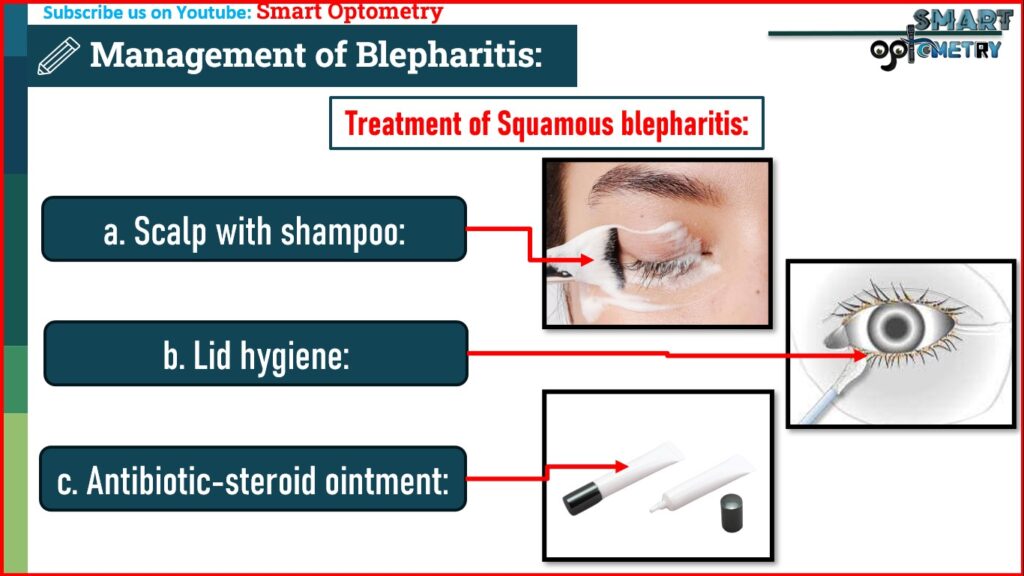
- a. Scalp with shampoo:
- Mainly, treatment of seborrheic dermatitis of the scalp by means of specific shampoo.
- b. Lid hygiene:
- Scales on eyelid margins is removed by a moistened cotton-tip applicator twice daily.
- c. Antibiotic-steroid eye ointment:
- Antibiotic-steroid eye ointment is applied locally, twice daily for 2–4 weeks.
Treatment of Ulcerative blepharitis:
Ulcerative blepharitis is severe form of blepharitis and need Local, Systemic & General treatments approach.
a. Local treatment

- Lid scrub:
- Warm sodium bicarbonate lotion (3%) is applied to the lid margin to soak the crusts.
- Alternately, a baby shampoo or 0.1% selenium sulphide solution may be used.
- Then removal of the crusts by a cotton-tip applicator.
- Epilation:
- Epilation of loose and diseased eyelashes.
- Antibiotic-steroid ointment:
- Antibiotic-steroid ointment is to be applied by rubbing the lid margins 3 times daily.
- Antibiotic drop or ointment is to be added.
- Chloramphenicol and ciprofloxacin are most effective against Staphylococcus aureus.
- Neomycin is best avoided because of high incidence of allergic reaction.
- If associated with dry eyes, use artificial tears 4 to 8 times daily.

b. Systemic therapy:
- Systemic tetracycline or doxycycline for two weeks is useful in severe form of ulcerative blepharitis.
- It is better avoided in children due to dental complications.
c. General treatment:
- Ocular hygiene and handwashing
- Avoid hair-oil, kajal or other ocular cosmetics
- Correction of refractive errors
- Treatment of seborrheic capitis by antidandruff shampoo
- Treatment of louse infestation.
.
.
What are the Complication of Blepharitis:
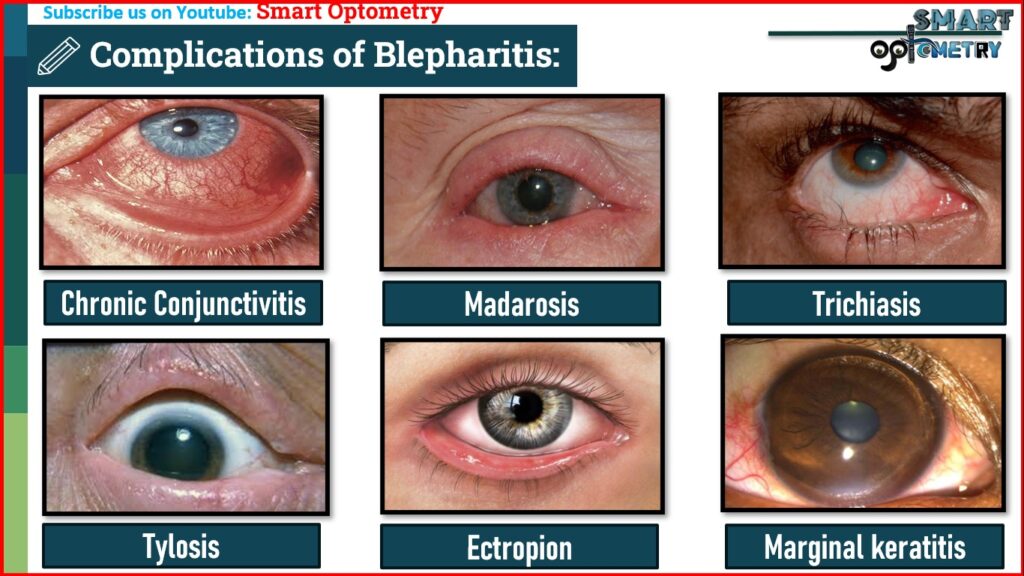
These are mainly seen in ulcerative form of blepharitis, and often serious.
1. Chronic Conjunctivitis:
Persistent inflammation in blepharitis can spread to the conjunctiva, leading to chronic conjunctivitis due to continuous irritation and bacterial infection.
2. Madarosis:
Loss of eyelashes is called Madarosis. Deep ulceration in ulcerative blepharitis destroys the hair follicles, resulting in the permanent loss of eyelashes and lead to madarosis.
3. Trichiasis:
Inward misdirection of cilia is called Trichiasis. When ulcers heal, scar tissue forms and contracts, pulling the remaining Cilia inward and causing Eyelashes to misdirect and rub against the cornea.
4. Tylosis:
Tylosis is a thickening of the tarsal border of the eyelid. Prolonged inflammation leads to thickening (hypertrophy) of the eyelid margins, causing them to droop, which can contribute to visual and functional discomfort.
5. Ectropion:
Outward turning of the lid margin is called ectropion. Scar tissue from healing ulcers can contract and pull the eyelid outward (ectropion), leading to poor tear drainage and epiphora (excessive tearing).
6. Marginal Keratitis:
Inflammation from blepharitis can extend to the corneal margin, particularly in the lower third, causing localized keratitis that may compromise corneal integrity.
7. Dry Eye:
Chronic inflammation disrupts the tear film, leading to its instability and subsequent dry eye symptoms due to insufficient or poor-quality tears.
- Check Our Courses: Ophthalmic Instrumentation, Clinical Refraction, Contact Lens, Binocular Vision, Dispensing Optics, MCQs in Optometry
- Download our App “Optometry Notes & MCQs” from Google Play Store.