Table of Contents
What is Ophthalmoscopy, Direct ophthalmoscopy & Indirect Ophthalmoscopy?

- Ophthalmoscopy is a clinical procedure performing using ophthalmoscope to examine interior structures of eye.
- There are two types of ophthalmoscope a) Direct Ophthalmoscope b) Indirect Ophthalmoscope.
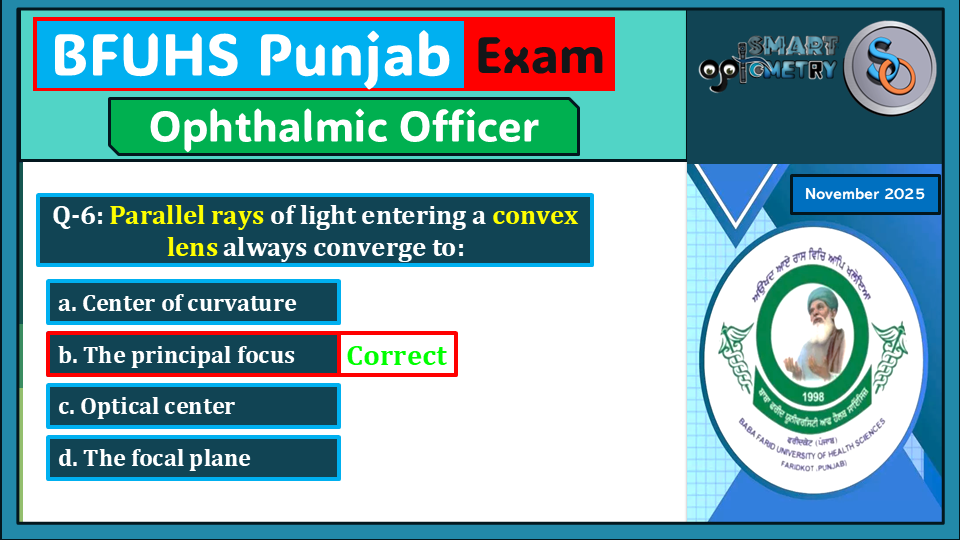
- In indirect ophthalmoscope an additional convex lens is required to see the fundus thus its called Indirect Ophthalmoscopy.
- In Direct Ophthalmoscope condensing lenses are incorporated inside the instrument that allow to see fundus without using any convex lens thus it’s called Direct Ophthalmoscopy.
- The ophthalmoscope was invented by Babbage in 1848, however its importance was not recognized, and it was reinvented by von Helmholtz in 1850.
Principle of Direct Ophthalmoscopy:
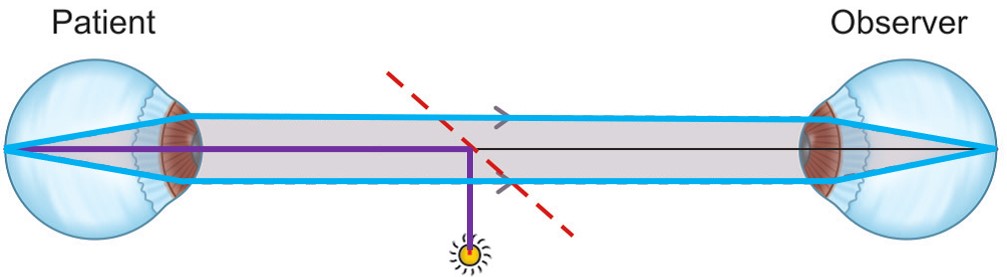
Direct ophthalmoscopy operates on the principle of utilizing a convergent beam of light that is directed into the patient’s pupil. This focused light then illuminates the interior structures of the eye, specifically the fundus. The emergent rays from any point on the patient’s fundus travel back through the pupil and reach the observer’s retina through the viewing hole of the ophthalmoscope.
In a perfect scenario, where both the patient and observer have normal refractive conditions (emmetropic), the emergent rays from the patient’s eye are parallel and are brought to focus on the observer’s retina without the need for additional correction, provided the observer’s accommodation is relaxed.
However, if either the patient or the observer (or both) has refractive errors (ametropia), adjustments are required to ensure proper focus and clarity. In such cases, a correcting lens is interposed between the observer and the ophthalmoscope. This correcting lens is determined by the sum of the patient’s and observer’s refractive errors. Modern ophthalmoscopes are equipped with a system of plus and minus lenses that allow for precise adjustment to compensate for any ametropia, ensuring that the emergent rays are properly focused on the observer’s retina.
Characteristics of Image formed in Direct Ophthalmoscope:
In direct ophthalmoscopy, the characteristics of the image formed are as follows:
1. Erect:
The image produced by a direct ophthalmoscope is upright or erect, meaning it is oriented in the same way as the actual structures within the eye. This characteristic allows for easier interpretation of the observed features, as they appear in their natural orientation.
2. Virtual:
The image is virtual, which means it is formed behind the ophthalmoscope and is not a real image that can be projected onto a surface. Instead, the observer views the virtual image through the ophthalmoscope’s viewing aperture or lens system.
3. Magnification:
The image is magnified approximately 15 times in emmetropic individuals, although this magnification may vary depending on the refractive condition of the observer and the patient. Generally, myopic individuals may experience greater magnification, while hyperopic individuals may experience less.
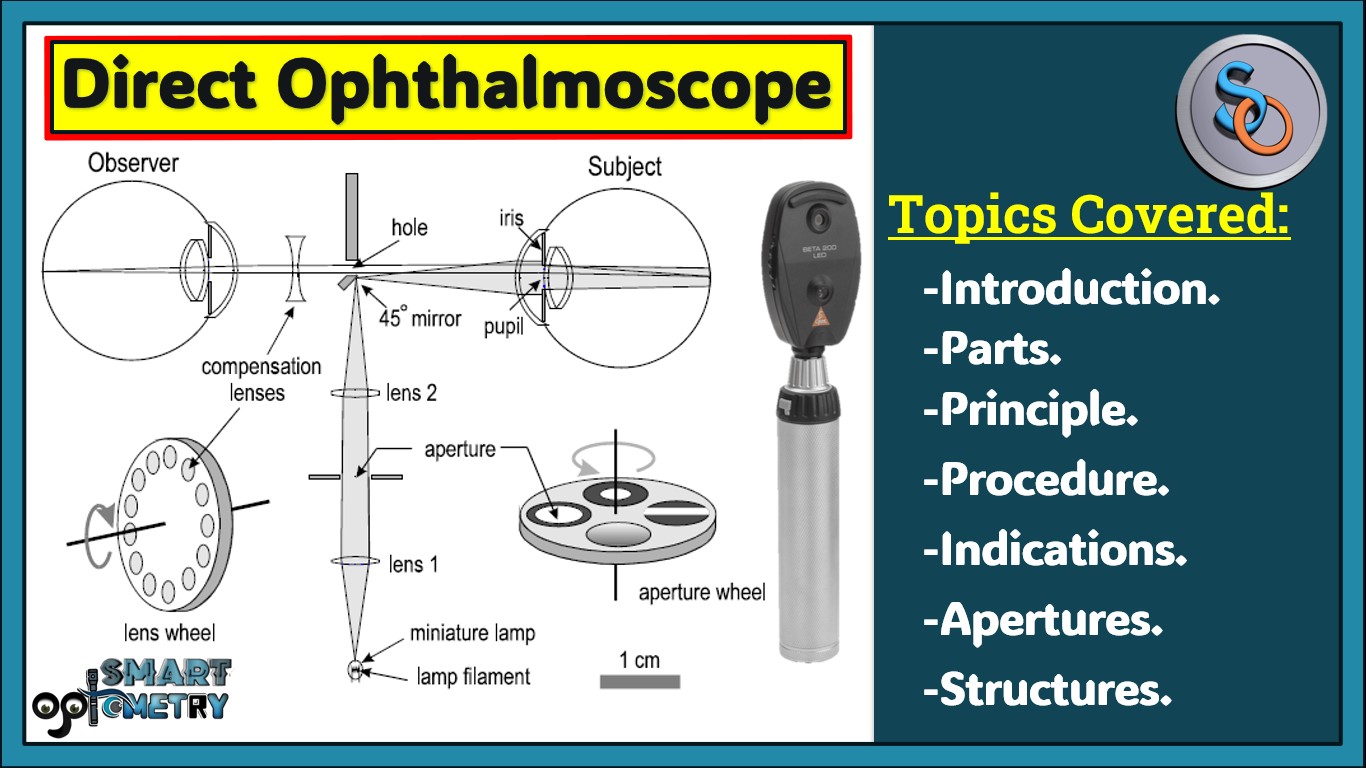
Structure of Direct Ophthalmoscope:
Structure of Direct Ophthalmoscope can be divided into 2 parts:
- The Illumination system.
- The Viewing System.
A. The Illumination system.
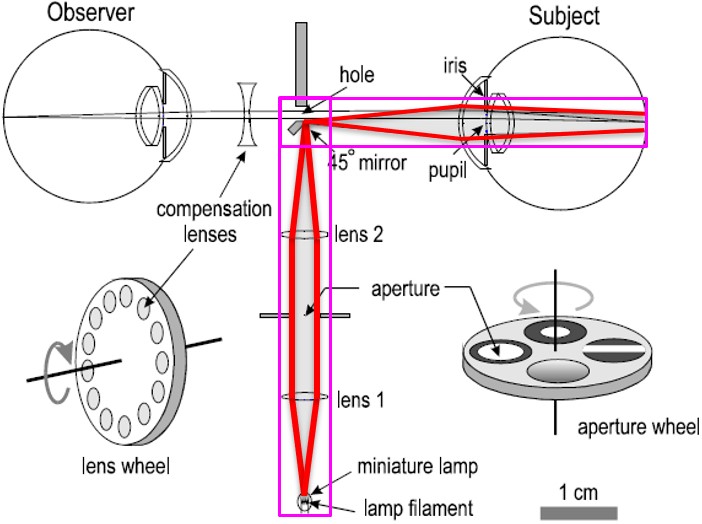
The illumination system of a direct ophthalmoscope serves to deliver light into the subject’s eye for examination of the interior structures. It comprises several components, each playing a specific role:
1. Electric Incandescent Lamp:
This serves as the light source for the ophthalmoscope. Light rays emitted from the lamp are initially slightly converged by Lens 1. Subsequently, Lens 2 focuses these rays to form an image of the lamp filament on the small 45° mirror.
2. Aperture:
Positioned between Lens 1 and Lens 2, the aperture allows for the selection of different shapes or colors of illumination. These apertures are conveniently mounted on a thumb-wheel, enabling easy interchangeability for various examination needs.
3. Two Lenses:
Lens 1 and Lens 2 are integral to the convergence and focusing of light rays emitted from the lamp. Lens 1 slightly converges the rays, while Lens 2 further focuses them to create an image of the lamp filament on the mirror.
4. Small 45° Mirror:
Positioned to receive the focused rays from Lens 2, this mirror plays a crucial role in directing the light into the subject’s eye. Light rays reflected by the mirror diverge, forming a cone-shaped bundle of rays that enter the eye. This bundle of rays traverses through the cornea and anterior chamber, with some being obstructed by the iris, while others pass through the pupil to illuminate the retina for examination.
B. The Viewing System.
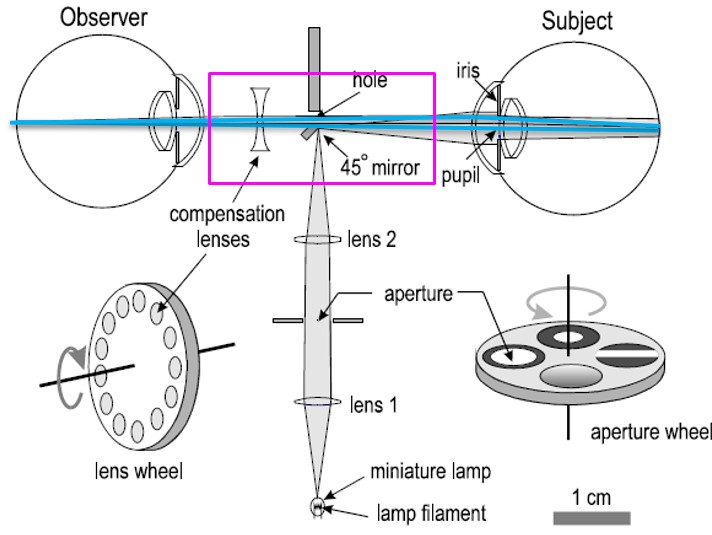
The viewing system of a direct ophthalmoscope enables the observer to visualize the light reflected from the subject’s eye, particularly focusing on the fundus for examination. It consists of several key components:
1. Viewing Hole:
Light rays initially reach the patient’s retina, where they reflect off the vitreous humor, crystalline lens, anterior chamber (AC), and cornea. These reflected rays then travel through the viewing hole of the ophthalmoscope, entering the observer’s eye.
2. Formation of Fundus Image:
As the bundle of reflected rays from the patient’s retina enters the observer’s eye, they strike the observer’s retina. This interaction results in the formation of an image of the patient’s fundus on the observer’s retina. This image allows the observer to visualize and examine the structures of the patient’s fundus, including the optic disc, macula, and retinal vessels.
3. Compensating Lenses:
Small diameter compensating lenses are positioned just behind the viewing aperture. These lenses serve to adjust the focus of the image from the subject’s retina, particularly if the subject is not emmetropic (i.e., if they have refractive errors). By using these compensating lenses, the observer can bring the image into sharp focus, ensuring clear visualization of the fundus structures for accurate examination.
Procedure of Direct Ophthalmoscopy:
The procedure of direct ophthalmoscopy involves several steps to ensure accurate examination of the patient’s fundus. Here’s a precise explanation based on the provided information:
1. Preparation of Room:
The examination room should be semi-dark to optimize visualization of the patient’s fundus.
2. Patient Explanation:
Before beginning the procedure, explain the steps to the patient. Inform them that you will need to get close to their eyes to see the retina clearly.
3. Consideration of Mydriatic Use:
If mydriatic drops were used to dilate the pupil for better visualization of the fundus, explain to the patient the potential consequences, such as temporary blurriness of vision and sensitivity to light. Ensure they understand these effects before proceeding with the examination.
4. Patient Positioning:
Ask the patient to sit comfortably and look straight ahead. The observer can either stand or sit slightly to the side of the eye being examined. For example, if examining the patient’s right eye, the observer should position themselves to use their right eye.
5. Observation and Illumination:
Using the direct ophthalmoscope, focus through the viewing hole and direct the beam of light into the patient’s pupil. Look for the red reflex, which indicates proper alignment and illumination.

6. Close Examination:
Once the red reflex is visible, move as close to the patient’s eye as possible to achieve optimal focus. Systematically examine the details of the retina, starting with the optic disc, blood vessels, the four quadrants of the general background, and finally, the macula.
7. Use of Compensation Lenses:
If either the patient or observer is not emmetropic (i.e., they have refractive errors), compensate for this by using the appropriate compensation lenses. Plus and minus lenses can be incorporated into the ophthalmoscope to ensure that the light rays focus correctly on the observer’s retina, enabling clear visualization of the fundus.
Apertures available in Direct Ophthalmoscope:
The direct ophthalmoscope offers various apertures, each tailored to specific examination needs. Here’s a precise explanation of the available apertures:
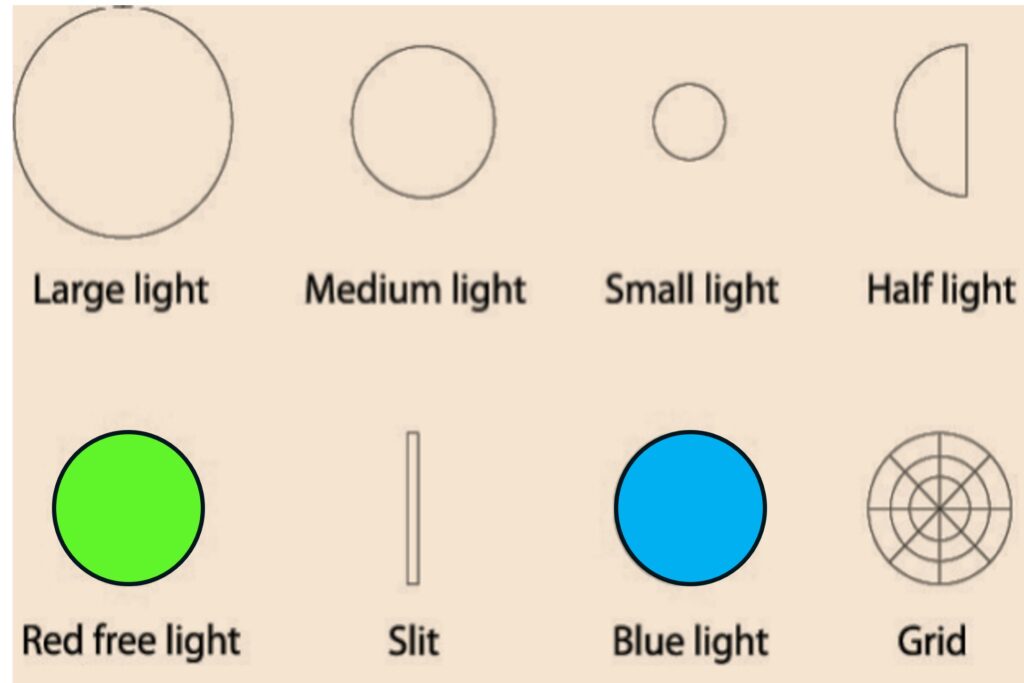
1. Large & Small Circle Light Source:
- Small Circle: Utilized when the pupil is very constricted, such as in cases without dilation.
- Large Circle: Recommended when mydriatic eye drops have been used to dilate the pupil.
2. Half Circle Light Source:
This aperture is beneficial if the pupil is partially obstructed by a lens with cataracts. It allows light to pass through only the clear portion of the pupil, preventing light from reflecting back.
3. Red Free:
Designed to enhance visualization of vessels and hemorrhages by improving contrast. This setting renders the retina in black and white, enhancing the clarity of vascular structures.
4. Slit Beam:
Used for examining contour abnormalities of the cornea, lens, and retina. It provides a narrow beam of light suitable for detailed assessment of these structures.
5. Blue Light:
Some ophthalmoscopes are equipped with a blue light feature, which is particularly useful for observing corneal abrasions and ulcers after fluorescein staining. The blue light enhances the visibility of these lesions.
6. Grid:
This aperture is employed for making rough approximations of the relative distance between retinal lesions. It is also utilized in visuoscopy to identify eccentric fixation, aiding in the assessment of visual function.
Indications of Direct Ophthalmoscopy:
Direct ophthalmoscopy is a valuable diagnostic tool with several indications for its use. Here’s a precise explanation based on the provided information:
1. Diagnosis of Opacities in Refractive Media:
Direct ophthalmoscopy enables the detection of opacities within the refractive media of the eye. These opacities appear as black shadows in the red glow seen through the ophthalmoscope, aiding in the diagnosis of conditions such as cataracts or corneal opacities.
2. Bruckner Test:
The Bruckner test, performed using direct ophthalmoscopy, provides insight into the refractive status of the eye without the need for retinoscopy. This test can help identify refractive errors and guide further assessment and management.
3. Assessment of Cup-Disc Ratio in Glaucoma:
Direct ophthalmoscopy allows for the evaluation of the cup-disc ratio, which is important for the early detection of glaucoma. Changes in the cup-disc ratio can indicate optic nerve damage, prompting further evaluation and management.
4. Visuoscopy:
Direct ophthalmoscopy with a grid aperture facilitates visuoscopy, which is useful for identifying eccentric fixation. This technique aids in the assessment of visual function and can be valuable in diagnosing and managing Amblyopia or eccentric fixation training.
5. Differentiation of Iris Mole and Hole:
Direct ophthalmoscopy aids in distinguishing between a mole and a hole in the iris. While a mole appears black as usual, a red reflex is observed through a hole in the iris during distant direct ophthalmoscopy, aiding in accurate diagnosis.
6. Recognition of Detached Retina or Fundus Tumors:
Distant direct ophthalmoscopy helps recognize signs of a detached retina or tumors arising from the fundus. A grayish reflex observed during examination may indicate the presence of these conditions, prompting further evaluation and management.
- Check Our Courses: Ophthalmic Instrumentation, Clinical Refraction, Contact Lens, Binocular Vision, Dispensing Optics, MCQs in Optometry
- Download our App “Optometry Notes & MCQs” from Google Play Store.



2 Comments
Stay with Smart Optometry and Study Optometry Smartly
I appreciate it a lot! 💯