Dry Eye treatment consists of a. Tear Substitute, b. Punctal Occlusion, c. Anti-inflammatory drugs, d. Contact Lens, e. Environmental, and f. Miscellaneous. We will know details about these in this post.
Dry eye syndrome, a condition affecting millions worldwide, can be a relentless source of discomfort and frustration. While its causative processes are often irreversible, managing symptoms and preventing surface damage is paramount. Here, we delve into a comprehensive approach to treatment, tailored to various levels of severity, as outlined by the Dry Eye Work-Shop (DEWS).
I. Strategy for Dry Eye Treatment
- The causative processes of dry eye are generally not reversible, and management is therefore control of symptoms and the prevention of surface damage.
- According to DEWS (Dry Eye Work-Shop) suggested treatment options depend on the level of severity of disease graded from 1 to 4.
II. Tear substitutes in Dry Eye Treatment:
- Tear substitutes have a relatively simple formulation that cannot approximate the components and structure of the normal tear film.
- There are no mucus substitutes and paraffin is only an approximation to the action of tear lipids.
Available forms are:
a. Drops and gels:
- Cellulose derivatives
- Hypromellose,
- Carbomer gels
- Methylcellulose
- Adhere to the ocular surface and so are longer-lasting.
- Polyvinyl alcohol (PVA)
- he persistence of the tear film and is useful in mucin deficiency.
- Diquafosol:
- Newer agent that works as a topical secretagogue
b. Ointments
- Containing petrolatum (paraffin) mineral oil can be used at bedtime to supplement daytime drops.
c. Eyelid sprays
- Contain a liposome-based agent that may stabilize the tear film and reduce evaporation.
d. Artificial tear inserts
- Emplaced once or twice daily offer extended duration treatment and are preferred by some patients.
e. Mucolytic agents
- Acetylcysteine 5% drops may be useful in patients with corneal filaments and mucous plaques.
f. Non-Preservative Drops:
- Numerous non-preserved drops are now available, including some multi-dose products.
III. Punctal occlusion in Dry Eye Treatment
- Punctal occlusion reduces drainage and thereby preserves natural tears and prolongs the effect of artificial tears.
- It is of greatest value in patients with moderate to severe Dry eye who have not responded to frequent instillation of topical agents.
- Punctal occlusion are of three types:
- 1. Temporary occlusion
- 2. Reversible prolonged occlusion
- 3. Permanent occlusion
IV. Anti-inflammatory agents in Dry Eye Treatment:
a. Topical steroids:
- Low-intensity preparations such as fluorometholone.
b. Omega fatty acid supplements:
- Omega-3 fish oil,
- Flax seed oil
C. Oral tetracyclines:
- To control associated blepharitis, especially meibomianitis.
d. Topical cyclosporin:
- Reduces T-cell mediated inflammation of lacrimal tissue, resulting in an increase in the number of goblet cells and reversal of squamous metaplasia of the conjunctiva.
V. Contact lenses in Dry Eye Treatment:
a. Low water content HEMA lenses:
- May be successfully fitted to moderately dry eyes.
b. Silicone rubber lenses:
- That contain no water and readily transmit oxygen are effective in protecting the cornea in extreme tear film deficiency.
c. Occlusive gas permeable scleral lenses:
- Provide a reservoir of saline over the cornea and can be worn on an extremely dry eye with exposure.
VI. Optimization of environmental humidity:
- Reduction of room temperature
- Room humidifiers
- Moist chamber goggles or side shields to glasses
VII. Miscellaneous options:
a. Botulinum toxin injection:
- In the orbicularis muscle may help control the blepharospasm that often occurs in severe dry eye.
b. Oral cholinergic agonists:
- Pilocarpine and cevilemine may reduce the symptoms of and dry mouth in patients with Sjögren syndrome.
c. Submandibular gland transplantation:
- For extreme dry eye and may produce excessive levels of mucus in the tear film.
d. Serum eye drops:
- Autologous or umbilical cord serum, they may aid the healing of persistent epithelial defects.
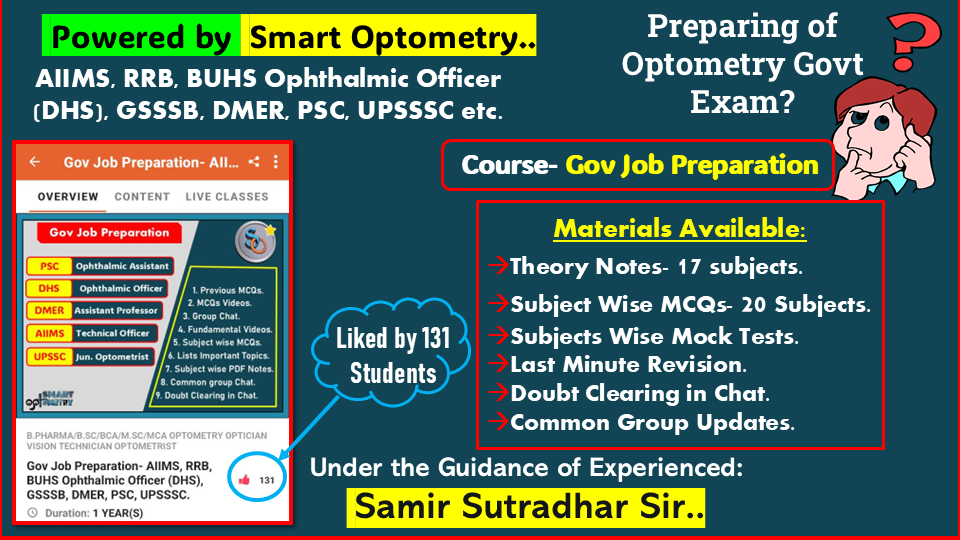
- Check Our Courses: Ophthalmic Instrumentation, Clinical Refraction, Contact Lens, Binocular Vision, Dispensing Optics, MCQs in Optometry
- Download our App “Optometry Notes & MCQs” from Google Play Store.