Gross Anatomy of Eyelids:
What is the definition of Eyelids?
- The eyelids are protective, mobile tissue curtains in front of the eyeballs.
- They act as shutters to shield the eyes from injuries, light, and help spread the tear film over the eye’s surface.
- Eyelids play a role in facial expressions and provide cues about a person’s wakefulness and attention.

Extend of Eyelids (Anatomy of Eyelids):
- Extent of Upper Eyelid:
- Extends downward from the eyebrow and forms the top boundary of the eye opening (palpebral fissure).
- Extent of Lower Eyelid:
- Extends upward to meet the skin of the cheek, creating the lower boundary of the eye opening.
Folds of Eyelid:
- Upper Eyelid Fold:
- Divides the eyelid into an orbital and a tarsal portion, formed by fibers from the levator muscle.
- Lower Eyelid Fold:
- Less prominent, marks the boundary between the eyelid and cheek area.
- Nasojugal and Malar Folds:
- These folds on the lower eyelid limit the spread of blood or fluid into the cheek.
.
.
Canthi/Canthus of Eyelids:
- Medial Canthus of Eyelids:
- The inner angle where eyelids meet, separated from the eyeball by the tear lake (lacus lacrimalis).
- Lateral Canthus of Eyelids:
- The outer angle, which lies in contact with the eyeball, forming an angle that changes with the eye’s opening.
Margins of Eyelids:
- Divided into a Medial Lacrimal Portion (rounded, no lashes, or glands) and a Lateral Ciliary Portion.
- The Grey Line marks the division between skin and conjunctiva, where lashes and meibomian gland openings are located.
Eyelashes of Eyelids:
- Arranged in 2-3 rows: Upper lid lashes (100-150) curve upward, lower lid lashes (50-75) curve downward to avoid interlocking when closed.
- Lashes are dark, fine-tapered, and renew every 3-4 months.
Palpebral Fissure of Eyelids:
- The elliptical space between the eyelids, which is approximately 28-30 mm horizontally and 9-11 mm vertically in adults.
- The alignment of the fissure can vary: some have a slight upward tilt (mongoloid slant), while others may tilt slightly downward (antimongoloid slant).
Associated Glands of Eyelids:
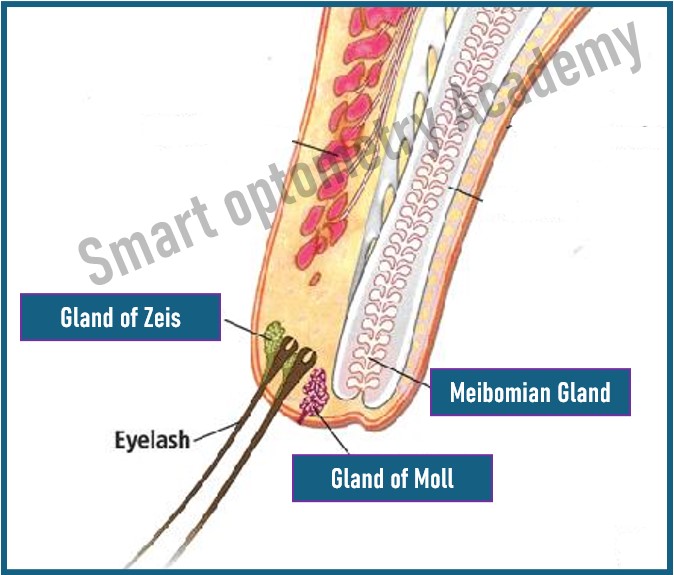
Glands of Zeis:
- Sebaceous glands that empty into the lash follicles.
Glands of Moll:
- Apocrine glands also associated with lash follicles, providing lubrication.
Note: These glands and lash follicles are highly sensitive, responding to touch for eye protection.
Anatomy/Structures of Eyelids:
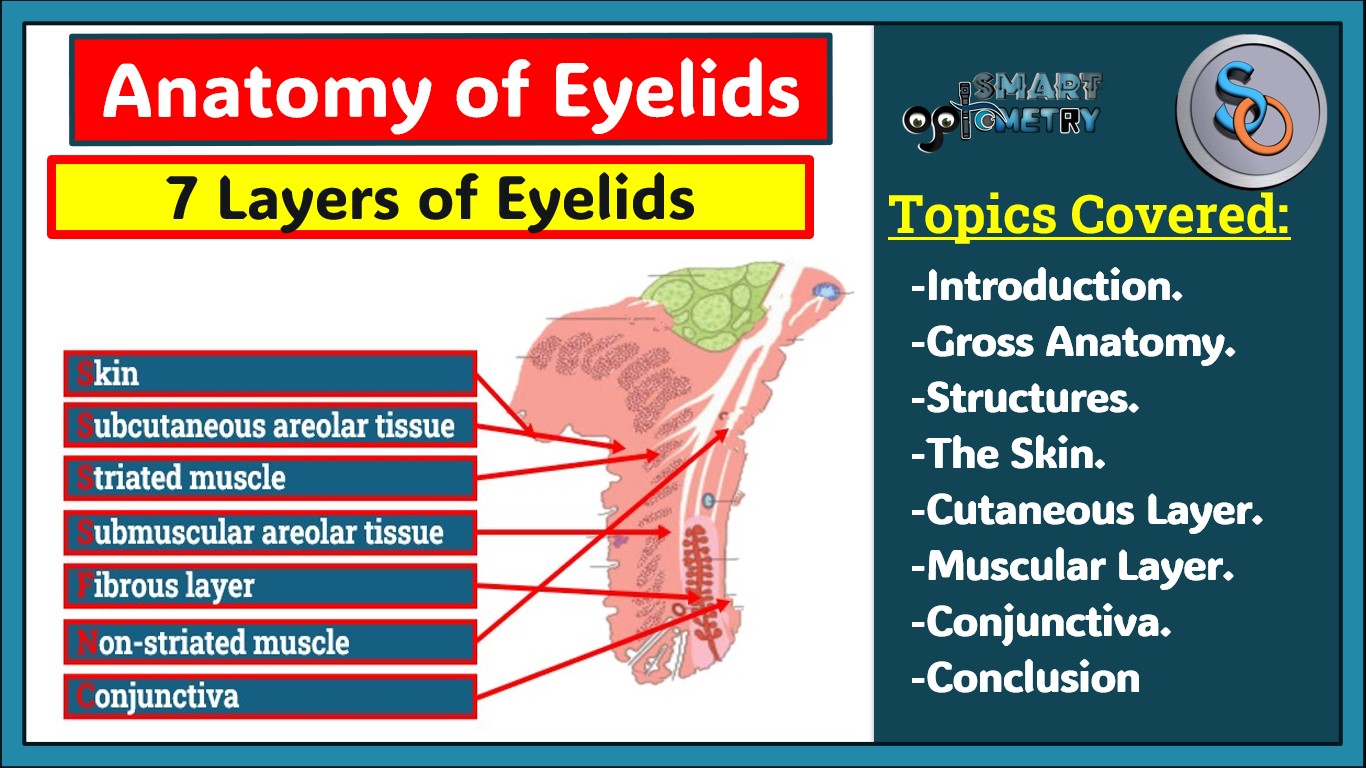
What are the Layers of Eyelids (Structures of Eyelids)?
- Eyelid has 7 layers:
- 1. Skin
- 2. Subcutaneous areolar tissue
- 3. Striated muscle
- 4. Submuscular areolar tissue
- 5. Fibrous layer
- 6. Non-striated muscle
- 7. Conjunctiva

Note: The skin on our eyelids is the thinnest in the entire body
- You can easily remember those layers by the mnemonic
“Smart Students Study Subjects For New Concepts”
- Smart = Skin,
- Students = Subcutaneous areolar tissue,
- Study = Striated muscle,
- Subjects = Submuscular areolar tissue,
- For = Fibrous layer,
- New = Non-striated muscle, and
- Concepts = Conjunctiva.
.
.
1. Skin of Eyelids (Structures of Eyelids):
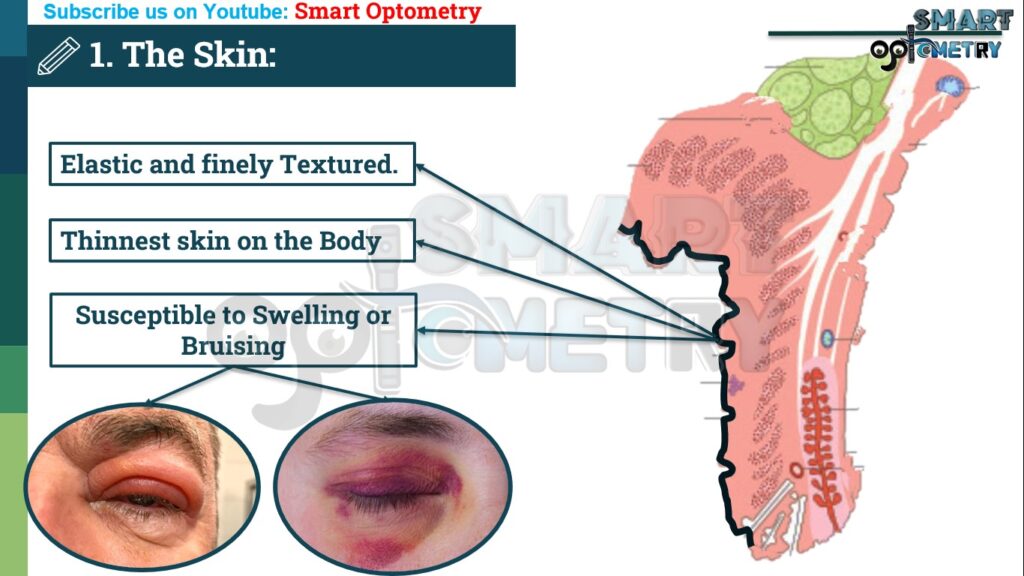
- The eyelid skin is the thinnest on the body, very elastic, and allows the eyelids to move quickly.
- The nasal skin (near the nose) is smoother and oilier than the skin on the outer part of the eyelid.
- Microscopic Structure: It consists of several layers of cells (epidermis), including a protective outer layer, and a dermis layer that has connective tissue, blood vessels, lymphatics, and nerves.
- The skin’s pigment can darken with chronic swelling or irritation.
2. Subcutaneous Areolar Tissue layer of Eyelids (Structures of Eyelids):
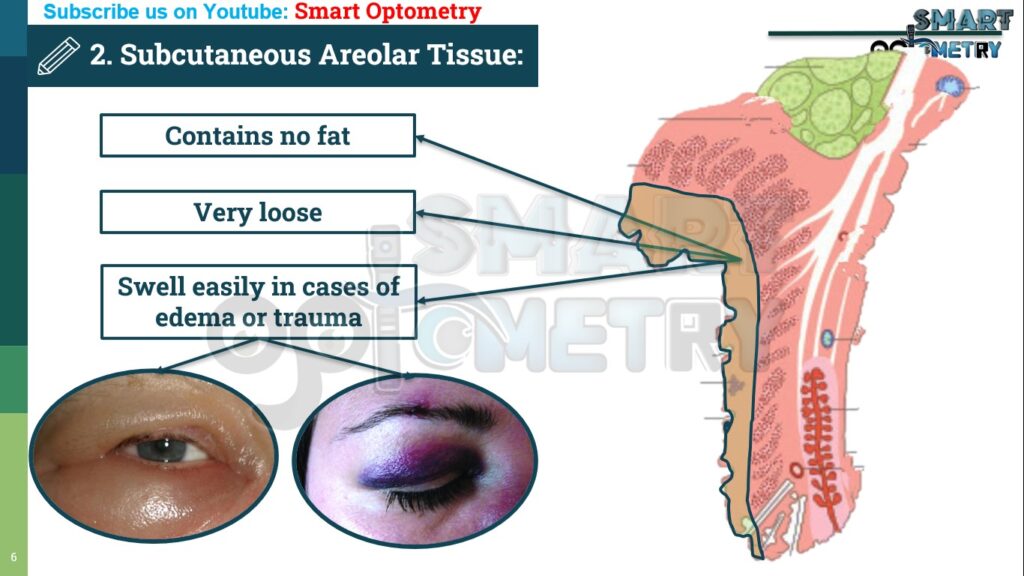
- A layer of loose connective tissue just below the skin with no fat, allowing easy movement of the skin.
- This layer can swell with fluid or blood, and it’s also helpful for eyelid surgeries.
- Not present near the lash line or where skin attaches to ligaments at the eyelid edges.
.
.
3. Striated Muscles layer of Eyelids (Structures of Eyelids):
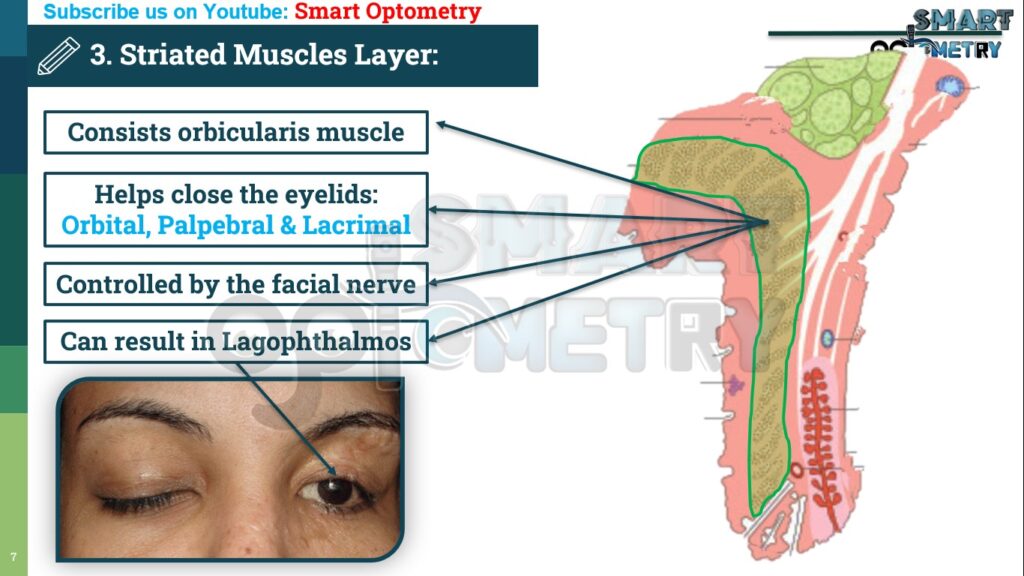
- This layer consists of orbicularis muscle which forms an oval sheet across the eyelids. In addition, the upper eyelid also contains levator muscle.
Orbicularis Oculi Muscle:
- This muscle encircles the eyelid and has two main parts:
Orbital Part of Orbicularis Oculi Muscle:
- Helps close the eyelid tightly and supports eyebrow movement.
Palpebral Part of Orbicularis Oculi Muscle:
- Helps in gentle eyelid closure, such as blinking or during sleep.
- This part is further divided into:
Preseptal and Pretarsal Portions of Orbicularis Oculi Muscle:
- Important for tear drainage and keeping the lids close to the eye.
Levator Palpebrae Superioris Muscle (LPS):
- Only in the upper lid, this muscle lifts the upper eyelid.
- Its tendon, called the aponeurosis, helps form the upper lid fold and connects to various points in the eyelid structure.
.
.
4. Submuscular Areolar Tissue layer of Eyelids (Structures of Eyelids):

- A loose tissue layer between the muscles and deeper structures, containing blood vessels and nerves.
- It splits the eyelid into front and back sections, allowing for easy surgical access.
- In the upper eyelid, it has two spaces (pretarsal and preseptal), separated by the levator muscle.
- These spaces allow movement and house blood supply.
.
.
5. Fibrous Layer of Eyelids (Structures of Eyelids):

- The fibrous layer forms the structural support of the eyelids and includes:
a. Tarsal Plate:
- This is the dense, fibrous tissue that gives the eyelid its shape and rigidity.
- It’s about 29 mm in length, with the upper tarsus being larger than the lower.
Surfaces of Tarsal Plate:
- The front (anterior) surface is convex and separates from the orbicularis muscle, allowing smooth movement.
- The back (posterior) surface curves to align with the eye.
Borders of Tarsal Plate:
- The edges provide attachment points for key structures like the orbital septum and muscles.
b. Septum Orbitale (Palpebral Fascia):
- A thin membrane that moves with the eyelids, linking the tarsal plates with the orbital rim.
Attachments and Relations of Septum Orbitale:
- Attaches to the tarsal plate centrally and to the orbital bone peripherally, allowing it to act as a barrier for orbital fat and connect with the surrounding muscle structures.
c. Medial and Lateral Palpebral Ligaments:
Medial Ligament:
- Attaches to the frontal bone, providing support and anchoring the eyelids at the inner corner of the eye.
Lateral Ligament:
- Anchors to the outer corner, connecting the tarsal plates with the orbital margin, ensuring stability during movement.
.
.
6. Non-Striated Muscle Fibers layer of Eyelids (Structures of Eyelids):
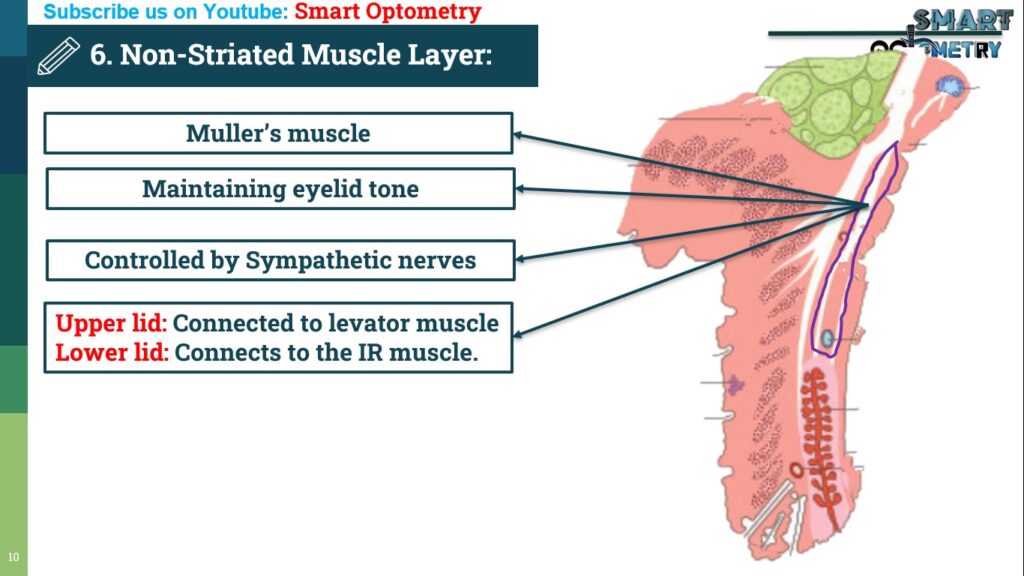
- This layer consists of Müller’s muscles (smooth muscle fibers), which are controlled by the sympathetic nervous system:
Location and Function of Non-Striated Muscle Fibers layer of Eyelids:
- Found in both upper and lower eyelids, just beneath the septum orbitale.
- They help elevate the upper eyelid and slightly lower the lower eyelid.
Sympathetic Control of Non-Striated Muscle Fibers layer of Eyelids:
- Stimulates lid retraction (pulls eyelids up).
- If damaged, it can lead to conditions like Horner’s syndrome, where the lid droops due to reduced muscle tone.
.
.
7. Conjunctiva of Eyelids (Structures of Eyelids):

- The conjunctiva is the innermost layer of the eyelid:
Structure and Location Conjunctiva of Eyelids:
- A thin mucous membrane that extends from the inner lid margin to the conjunctival fornix, covering the back of the tarsal plate and Müller’s muscle.
Function Conjunctiva of Eyelids:
- Provides a protective barrier and helps produce mucus to keep the eye moist.
- Check Our Courses: Ophthalmic Instrumentation, Clinical Refraction, Contact Lens, Binocular Vision, Dispensing Optics, MCQs in Optometry
- Download our App “Optometry Notes & MCQs” from Google Play Store.