Table of Contents
What is Myopia?
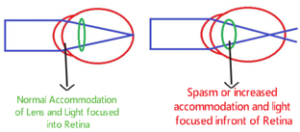
- The refractive condition in which parallel light rays from an object at optical infinity are focused by the eye in front of the retina, with accommodation relaxed.

- Myopia is a highly significant problem, not only because of its high prevalence, but also because it can contribute to visual morbidity and increase the risk for vision-threatening conditions (e.i, Retinal breaks and detachment, glaucoma).
- It can be a limiting factor in occupational choices.
- The posterior segment changes in the myopic eye place it at risk for the development of other ocular conditions.
- It is also called Near-sightedness.
Why myopic Patient can see clearer at near as compare to distance?
In myopia, the converging power of eyes increases which brings the far point of eyes close to eyes due to which myopic patients can see near clearly as compared to distance.
Prevalence of Myopia:
- The prevalence of myopia varies with age and other factors.
- When examined without the aid of cycloplegic agents, a significant number of infants are found to have some degree of myopia.
- Their myopia tends to decrease, and most such infants reach emmetropia by 2-3 years of age.
- The prevalence of myopia is high in premature infants.
- Some studies have found a slightly higher prevalence of myopia in females than in males.
- The prevalence of myopia increases with income level and educational attainment, and it is higher among persons who work in occupations requiring a great deal of near work.
Classifications of Myopia:
Etiological Classification of Myopia:
Axial myopia:
- Myopia Due to increased anteroposterior (axial) length of eye and others parameters are normal

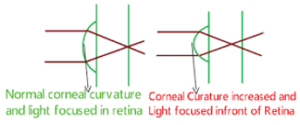
Curvature myopia:
- It occurs due to increased curvature of the cornea, lens or both.
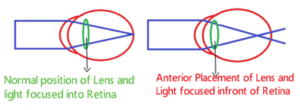
Positional myopia:
- It occurs due to anterior placement of crystalline lens in the eye.
Myopia due to excessive accommodation:
- It occurs in patients with spasm of accommodation. In spasm of accommodation Crystalline lens can’t able to relax (Lens remain in accommodative state) that leads to rays focus in front of the retina.
Index myopia:
- Due to increase in the refractive index of crystalline lens associated with nuclear sclerosis.
Clinical Classification of Myopia:
Simple myopia:
- The refractive status of the eye with simple myopia is dependent on:
- The optical power of the cornea
- The optical power of the crystalline lens, and
- The axial length.
- It’s a physiological abnormality, not associated with any disease.
- Simple myopia occurs due when
- Eyes are too long for its optical power, or
- Eyes are too optically powerful for its axial length.
- This is much more common than the other types of myopia and generally less than 6D
Nocturnal myopia:
- Nocturnal myopia occurs only in dim illumination, primarily due to increased accommodative response associated with low levels of light.
- Due to insufficient contrast, accommodations get stimulated and light focus in front of the retina.
Pseudomyopia:
- It occurs due to overstimulation of the eye’s accommodative mechanism or ciliary spasm.
- Due to overstimulation accommodation the total power of the eye increased and light rays focused in front of the retina.
Degenerative or pathological myopia
- A high degree of myopia associated with degenerative changes in the posterior segment of the eye.
- The degenerative changes can result in abnormal visual function:
- Decrease in best corrected visual acuity.
- Changes in visual fields.
Induced or acquired myopia:
- It occurs due to:
- Exposure to various pharmaceutical agents
- Variation in blood sugar levels
- Nuclear sclerosis of the crystalline lens
- This myopia is often temporary and reversible.
Classification of Myopia: (Degree of myopia)
- Low myopia (<3.00D)
- Medium myopia (3.00D – 6.00D)
- High myopia (>6.00 D)
Classification of Myopia: (Age of Onset)
Congenital myopia:
- Present at birth and persisting through infancy
Youth-onset myopia:
- It occurs before 20 years (<20 years of age)
Early adult-onset myopia:
- It occurs between 20-40 years of age (20-40 years of age)
Late adult-onset myopia:
- It occurs after 40 years of age (>40 years of age)
Clinical Features of myopia:
Symptoms of Myopia:
1. Simple Myopia:
- Blurred distance vision.
- Asthenopic symptoms: due to-
- Astigmatism.
- Anisometropia.
- Accommodative dysfunction.
- Vergence disorder.
- Half shutting of eye.
2. Nocturnal Myopia:
- Blurred distance vision:
- Only in dim illumination or in dark conditions.
- Difficulty in driving at night.
3. Pseudo Myopia:
- Blurred distance vision:
- May be constant or intermittent but significantly increase after near work.
4. Degenerative or pathological myopia:
- Blurred distance vision: blur is constant.
- Vitreous floaters:
- Due to degenerated liquefied vitreous
- Night blindness:
- if rods and cones are damaged
5. Induced myopia:
- Blurred distance vision:
- Lasting a few hours depending upon the particular agent or condition causing it.
Signs of Myopia:
1. Simple myopia:
- Reduced unaided distance visual acuity
- Large and prominent eyeballs
- Deep anterior chamber
- Sluggishly reacting pupil
- Fundus:
- Usually normal and rarely myopic crescent may be seen
- Magnitude of refractive error:
- Occur between 5 and 10 year of age and it keeps on increasing till about 18-20 years of age at a rate of about –0.5 ± 0.30 every year.
2. Pseudomyopia:
- Fluctuations in accommodation:
- Observable as variations in visual acuity and Retinoscopic reflex
- Cycloplegic refraction:
- More minus power on the manifest refraction than on the cycloplegic refraction.
3. Nocturnal myopia:
- Retinoscopy:
- Retinoscopy in a dark room may be shifted in the minus direction.
4. Degenerative or pathological myopia:

- Prominent eyeballs
- Cornea is large
- Anterior chamber is deep
- Large and sluggish pupils
- Visual field contraction
- Electroretinogram (ERG) :
- May be subnormal due to chorioretinal atrophy.
- Fundus sign:
- Large and pale optic disc.
- Tilted optic nerve with peripapillary atrophy.
- Temporal myopic crescent.
- Chorioretinal atrophy.
- Peripheral vitreous detachment.
- Lacquer cracks.
- Lattice degeneration Foster-fuchs spots.
- Peripheral retinal holes.
- Macular holes.
Investigations of Myopic Patient:
1. Visual Acuity:
- Both unaided distance and near visual acuities should be measured.
- Because of the correlation of unaided distance visual acuity with the degree of myopia.
- When the patient regularly wears an optical correction, aided visual acuity should be measured.
2. Ocular Motility, Binocular Vision, and Accommodation:
- Convergence excess, accommodative insufficiency, and accommodative infacility are frequently observed in patients with myopia.
- So testing should include assessment of:
- Accommodation,
- Vergence, and
- Binocularity.
3. Refraction:
Retinoscopy:
- Provides an objective measure of refractive error and provide a good approximation of the subjective refraction.
- Retinoscopy in a completely darkened room may be useful in the diagnosis of nocturnal myopia.
- A careful subjective refraction should be conducted to determine the lowest minus lens power that achieves best visual acuity.
Auto Refractometer:
- Objective Autorefractometer may be substituted for retinoscopy, although an autorefractor will not give the qualitative information, like:
- Clarity of the ocular media,
- Optical quality of the retinoscopic reflex, and
- Fluctuations in pupil size
Cycloplegic Refraction:
- Cycloplegic Refraction is required for the definitive diagnosis of pseudomyopia.
4. Keratometry:
- Keratometry can be useful in predicting the degree of any astigmatism.
5. Ocular Health Assessment:
- Ocular Health Assessment of the patient with myopia should include:
- Direct or indirect ophthalmoscopy
- Fundus biomicroscopy and
- Measurement of intraocular pressure.
6. Slit lamp Biomicroscopy:
- These testing is indicated risk of retinal and choroidal atrophy, and retinal breaks and detachment in patients with myopia.
- Viewing of the peripheral retina is enhanced by papillary dilation and is of particular importance in pathological myopia.
- Slit lamp biomicroscopy can be important in the differential diagnosis of:
- Induced or acquired myopia,
- Contact lens-induced corneal edema,
- Lenticular nuclear sclerosis.
Management of Myopia- Optical, Pharmacological, Surgical:
1. Optical Correction:
- Optical correction contain:
- Spectacles: Concave lens
- Contact Lenses
- Whether spectacles or contact lenses are preferable in a given case depends:
- Patient age
- Motivation for wearing contact lenses
- Compliance with contact lens care procedures,
- Corneal physiology
- Financial considerations
2. Medical (Pharmaceutical)
- Cycloplegic agents are sometimes used to reduce accommodative response as part of the treatment of pseudomyopia.
- Some studies have reported that daily topical administration of atropine and cyclopentolate reduces myopia progression rates in children with youth-onset myopia.
- Problems associated with cycloplegic agents are:
- Risks associated with chronic cycloplegia,
- Light sensitivity due to pupillary dilation,
- High plus lens additions(2.5D),
- Retinal adverse effects.
3. Vision Therapy:
- Unaided visual acuity can be improved in patients with myopia using vision therapy, but myopia does not appear to be reduced, it reduce myopic progression rates.
- Vision therapy to reduce accommodative response is often provided for pseudo myopia.
- Auditory biofeedback has also been used successfully in the treatment of pseudo myopia.
4. Orthokeratology:
- Orthokeratology is generally performed only on adults.
- In Orthokeratology a series of contact lenses, over a period of weeks or months, to flatten the cornea and reduce myopia.
- Studies shows that orthokeratology with standard rigid contact lenses can reduce upto 3D and average reduction 0.75D to 1D
- However, studies suggest that refractive error shifts toward the original baseline in patients who stop wearing contact lenses.
5. Refractive Surgery:
A. Corneal Based:
Radial keratotomy (RK):
- A spoke-like radial pattern of incisions in the paracentral cornea leaving central 4mm
- When incisions heals it makes the central cornea flattens.
- The amount of resultant refractive change depends on the size of the optical zone and the number and depth of the incisions.
- It can correct Upto 2-6D.
Photorefractive keratectomy (PRK):
- Central optical zone of anterior corneal stroma is photo ablated using excimer laser to cause flattening of cornea.
- It can correct upto mild to moderate myopia (2-6D).
Cryolathe keratomileusis:
- A section of corneal stroma is removed, frozen, and shaped on a lathe to minus power.
- It is then replaced in the cornea to reduce corneal power. Cryolathe keratomileusis is used for more severe myopia.
Automated lamellar keratomileusis (ALK):
- A layer of corneal epithelium and superficial stroma of predetermined thickness is removed with a microkeratome except for a small attachment to the cornea.
- The microkeratome is then used to remove a specific amount of corneal stroma to flatten the cornea after which, the flap of superficial corneal tissue is replaced.
Laser in situ keratomileusis (LASIK):
- In this technique, first a flap of 130-160 micron thickness of anterior corneal tissue is raised.
- After creating a corneal flap mid-stromal tissue is ablated directly with an excimer laser beam, ultimately flattening the cornea.
- It can correct myopia of up to – 12 D.
Intracorneal Ring Implantation (ICR):
- Ring implanted in 2/3 stromal depth cause cornea flatten.
- It can correct upto 12D
B. Lenticular Based:
Extraction of Clear Crystalline lens:
- Remove the crystalline lens and an artificial Intraocular Lens (IOL) is implanted
Phakic Intraocular Lens:
- Implantable collamer lens (ICL) is implanted in the anterior chamber and posterior chamber anterior to crystalline lens.
- It’s a reversible procedure and can correct upto 16-20D.
- Check Our Courses: Ophthalmic Instrumentation, Clinical Refraction, Contact Lens, Binocular Vision, Dispensing Optics, MCQs in Optometry
- Download our App “Optometry Notes & MCQs” from Google Play Store.